HARARE, Zimbabwe – Michelle and Michael Mutsvaki contracted HIV from their mother at birth, but while their parents have rejected antiretroviral (ARV) medication, the siblings have chosen treatment. The siblings, aged 22 and 24, learned about their HIV status from their mother, who assured them that their faith would protect them from the disease. However, they witnessed their father’s death from HIV complications a decade ago, despite relying on faith healers for treatment.
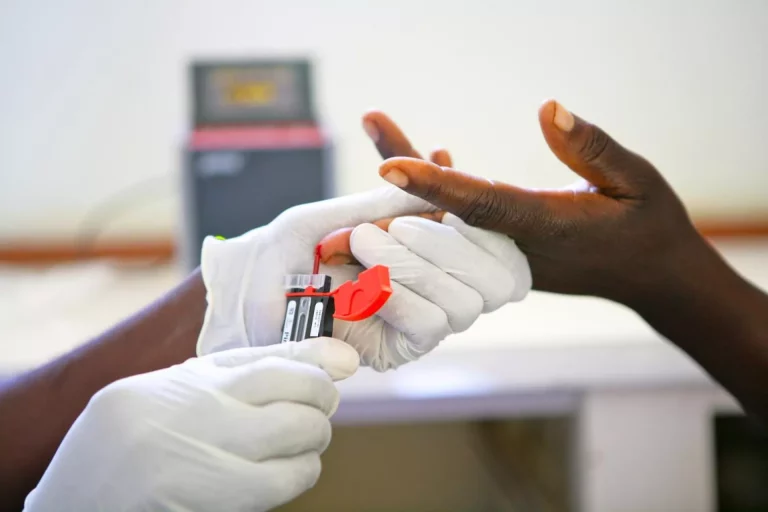
Their mother, a follower of the Johane Masowe Church, continues to rely on religious beliefs and remedies instead of taking ARVs. In contrast, Michelle and Michael made the crucial decision to start ARV treatment after learning about its importance from HIV/AIDS activists who visited their school in 2017. Despite being born at home without medical assistance due to their parents’ religious beliefs, they contracted HIV during birth, a risky time for newborns born to HIV-positive mothers due to exposure to body fluids.
Zimbabwe’s adult population has largely embraced HIV treatment, with 86.8% of adults living with HIV aware of their status and 97% of them receiving ARVs, according to the 2020 Zimbabwe Population-based HIV Impact Assessment Survey. However, there are still individuals like Susan Mutsvaki, Michelle and Michael’s mother, who openly reject ARVs due to their faith, relying on church remedies instead.
Hector Chinopa, who tested positive for HIV after contracting COVID-19 in 2020, has also refused ARVs, citing his lack of illness as a reason for avoiding treatment. Similarly, Linet Gavi, who tested HIV-positive two years ago, has not taken treatment and wonders if she transmitted the virus to her teenage sons, who passed away in 2019 from unknown causes.
Despite efforts by the Zimbabwean government to encourage HIV patients to seek treatment, individuals like Chinopa, Gavi, and Mutsvaki avoid government clinics and reject ARVs. The Global Fund has invested $1.8 billion in Zimbabwe’s HIV program between 2003 and 2022, with recent approval of a $437 million HIV grant for 2024-2026.
Although some Zimbabweans resist HIV treatment, late last year, 95% of the HIV-positive population achieved undetectable viral loads, making transmission unlikely. Additionally, Zimbabwe approved CAB-LA, a long-acting injectable medication for HIV prevention, becoming the first African country to do so. However, individuals like Chinopa, Gavi, and Mutsvaki remain steadfast in their refusal to participate in HIV treatment, contributing to AIDS-related deaths due to misinformation and myths surrounding ARVs.